SAN JOSE, California: Pacific Stroke Association (PSA) conducted its stroke awareness seminar, Ability Resource Forum, in two sessions in Redwood City, Silicon Valley, California September 17 and at the Valley Specialty Center in San Jose September 20.
It brought together experts such as doctors, occupational and speech therapists, acupuncture and natural health providers, stroke researchers and also survivors and caregivers of stroke victims.
A stroke is also called a “brain attack”. Most often, a stroke occurs when blood flow to the brain stops because it is blocked by a clot. The brain cells in the immediate area begin to die because they stop getting the oxygen and nutrients they need to function.**
Types of stroke: There are two types of stroke:
● Ischemic – the most common kind that is caused by a blood clot that blocks or plugs a blood vessel in the brain
● Hemorrhagic – This is caused by a blood vessel that breaks and bleeds into the brain**
 Stroke can cause mild to severe disabilities from problems with thinking and speaking and emotional problems to paralysis. It is critical to arriving at the hospital as soon as symptoms start – within 60 minutes – to minimize disability.
Stroke can cause mild to severe disabilities from problems with thinking and speaking and emotional problems to paralysis. It is critical to arriving at the hospital as soon as symptoms start – within 60 minutes – to minimize disability.
Symptoms include trouble in walking, seeing or speaking or weakness on one side. An acronym called FAST helps one to be aware of the symptoms – Face (sudden contortion of the face), Arm (losing sensation in one’s arm or sudden weakness), Speech (slurred speech), Time (Call emergency number 911 immediately).**
The first speaker was Cindy Johans, a clinical researcher in the field, who herself became a victim of a stroke. She led a very healthy lifestyle – she was a long-distance runner and triathlete – and did not smoke. She did not have high cholesterol either.
A fortunate set of circumstances led to her receiving timely medical help – a friend was visiting Cindy at her house when it happened. Her own clinical research background helped Cindy discern that she was having a stroke. She was rushed to the emergency room (ER). Post-stroke, her friends were her local support system. Physical therapy helped her recover and she is now, in her own words, about “85-90 per cent normalized”.
Cindy said she feels grateful for having had that experience from the patient’s side. “I didn’t know what stroke victims go through.” Dr Maarten Lansberg, MD, an associate professor in neurology at Stanford University Medical Center, spoke on current topics in stroke rehabilitation.
In his words, these were the ingredients in the “recipe for the best possible recovery, better than any medicine”: motivation and willingness to work hard; an optimistic outlook in life; and support from family and friends
“Your brain can still learn after stroke,” Dr Lansberg said. “Some of it is not always logical. For example, a patient may say, ‘I started working on a stationary bike and my speech improved’.”
He gave a summary of different therapies used in stroke rehabilitation, including modern technological advances.
Kathy Bermejo, a certified brain injury specialist at the Center for NeuroSkills (neuroskills.com), spoke on the subject of cognitive fundamentals and brain Injury.
In the broadest sense of the word, cognition refers to attention, memory, decision-making and categorization of different terms, people and objects.
A brain injury can impact a lot of different cognitive processes such as:
– Decision-making
– Filtering out distractions
– Recognizing simple objects such as an apple
– Routine daily activities
“We often take our daily activities for granted. However, without having these automatic processes down, one can’t do hierarchical tasks,” Bermejo said. “We have to treat all these skills, we can’t treat in isolation.”
Stroke is not something that only affects people beyond a certain age. Bermejo recently evaluated a nine-year-old. “Strokes are happening in younger people all the time,” she said.
Pharmacological treatments (medications) help in recovery, too. Dr Jeffrey Krauss, a rehab specialist at the VA (Veterans’ Administration), Palo Alto, California, spoke on the multi-disciplinary subject of lifestyle medicine as both a preventive measure and treatment after stroke.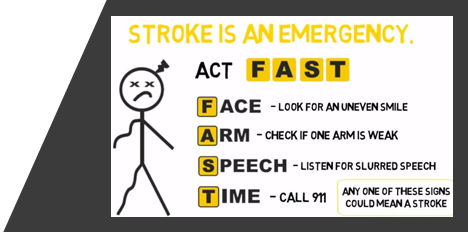
Lifestyle medicine focuses on diet, exercise, substance moderation, sleep, stress management and social connections, or as Dr. David Katz of Yale University said, “Feet, fork, fingers, sleep, stress and love.”
Dr Krauss referred to a cardiac rehabilitation study conducted by the famous physician, Dr Dean Ornish, which found that arteries could be unclogged by following a lifestyle that incorporates the above elements.
There is a correlation between stroke and certain health conditions: cardiovascular disease (75 per cent), depression and anxiety (14 to 94 per cent), and high systolic blood pressure, the number one risk factor. In general, there is a high risk of recurrence in the first five years following an initial stroke. Around 52-59 per cent of ischemic strokes are preventable by adhering to a healthy lifestyle.
While medications are helpful, exercise helps in improving neuroplasticity – the ability of the brain to learn new things by forming new neural connections. Neuropsychologist Dr Mahnaz Moteyar spoke about humanizing the patient experience.
“We have a medical system, not a community,” Dr Moteyar said. “By bringing in creativity, we can make rehab a joyous experience.” She talked about the importance of language in framing the whole patient experience. For example, she pointed out that instead of using the term, “suffered from a stroke”, one can use “experienced a stroke”.
Her opinion on the current clinical language is that it creates a “neuroplasticity that is disempowering and destabilizing.”
She emphasized the importance of compassion in the healing process and of passion (desire to heal), purpose and patience. Dr Roberta Wang, associate chief of brain injury and stroke rehabilitation in the Department of Physical Medicine and Rehabilitation at Santa Clara Valley Medical Center, spoke on the topic of reintegrating the patient back into society.
She stressed on the importance of social support in recovery, saying that the best outcomes were to be found with moderate instrumental (physical) support and high emotional support. Pets are important, too. Dr Wang spoke about the psychological and recreational therapists that are part of her hospital’s program.
“The things that make life really meaningful are not quantifiable,” she said. Post-stroke recovery can involve areas such as the patient’s sexuality and the relationship with his/her partner. Many abilities are impaired such as driving, which impact returning to work. Dr Wang concluded with admiration for her patients and said: “We are always humbled by the patients and their families. It is a privilege to be involved in this stage of recovery.”